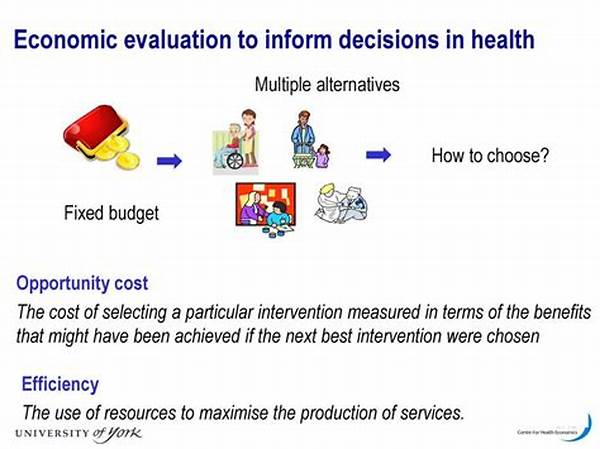
The ever-evolving landscape of health services necessitates a rigorous approach to managing scarce resources and maximizing patient outcomes. Economic evaluation in health services serves as a pivotal tool in achieving these goals. This analytical approach encompasses the assessment of costs and outcomes associated with healthcare interventions, enabling policymakers to make informed decisions. By systematically comparing different strategies, economic evaluation aids in optimizing the allocation of resources in healthcare settings and ensures that the most effective treatments are prioritized.
Read Now : Enhancing Customer Service With Apis
The Importance of Economic Evaluation in Health Services
In the realm of healthcare management, understanding the intricacies of economic evaluation is crucial for achieving sustainable health outcomes. Economic evaluation in health services provides a framework for assessing the value of various health interventions. It involves methodologies such as cost-effectiveness analysis, cost-utility analysis, and cost-benefit analysis. These methodologies allow healthcare providers and decision-makers to weigh the benefits and costs of different treatments and interventions systematically.
By incorporating economic evaluation in health services, healthcare systems can make evidence-based decisions that promote efficiency and effectiveness. The importance of this approach is underscored by the growing demand for transparent and accountable healthcare practices. As healthcare budgets become increasingly constrained, employing economic evaluations ensures that health services deliver maximum value for the resources invested. Ultimately, economic evaluation serves as a cornerstone for informed, equitable, and sustainable health systems.
Key Methodologies in Economic Evaluation in Health Services
1. Cost-Effectiveness Analysis: A method to compare the relative expenses and outcomes of different interventions. Economic evaluation in health services utilizes this to determine which treatments provide the best value for money within the healthcare budget constraints.
2. Cost-Utility Analysis: This approach incorporates patient preferences and quality of life into the evaluation. Economic evaluation in health services uses cost-utility analysis to assess interventions based on the quality-adjusted life years (QALYs) produced.
3. Cost-Benefit Analysis: An approach that values both costs and outcomes in monetary terms. Economic evaluation in health services employs cost-benefit analysis to ascertain the net economic gain from healthcare interventions.
4. Budget Impact Analysis: This analysis evaluates the financial implications of adopting new interventions on a healthcare budget. Economic evaluation in health services requires budget impact analysis to assess fiscal sustainability.
5. Decision-Analytic Modeling: A technique that uses mathematical modeling to forecast outcomes under varying scenarios. Economic evaluation in health services often depends on decision-analytic modeling to anticipate the long-term impacts of healthcare decisions.
Challenges and Opportunities in Economic Evaluation in Health Services
While economic evaluation in health services offers significant benefits, it also presents challenges. One primary challenge is the complexity of accurately measuring costs and outcomes. Diverse patient populations and varying healthcare settings contribute to these complexities. Moreover, the integration of economic evaluation into policy decision-making processes is often hindered by political and institutional barriers.
Despite these challenges, opportunities abound. Advances in data analytics and improved access to health economics training can enhance the precision and applicability of economic evaluations. Furthermore, collaboration between economists, healthcare providers, and policymakers can foster an environment conducive to employing these evaluations effectively. Embracing economic evaluation in health services as a standard practice can lead to more informed and transparent healthcare systems, benefiting patients and society as a whole.
Real-World Applications of Economic Evaluation in Health Services
Economic evaluation in health services is not only theoretical but increasingly used in real-world settings to influence policy and practice. It helps prioritize interventions that provide substantial health benefits relative to their costs. In numerous instances, economic evaluation has redirected funding from less effective treatments to interventions with greater impact.
Read Now : Data Integration Best Practices
This practice significantly contributes to health technology assessments (HTAs), which governments globally rely on for funding decisions. By applying economic evaluation in health services, HTAs aid in ensuring that the resources are channeled towards interventions that drive actual improvements in population health. Through rigorous assessments, these evaluations serve as a foundational component in formulating health policies, optimizing resource allocation, and enabling equitable healthcare access.
Integrating Economic Evaluation into Health Policy Development
The incorporation of economic evaluation in health services into policy development is vital for shaping sustainable healthcare frameworks. Policymakers utilize these evaluations to differentiate between interventions that are both clinically effective and cost-efficient. Additionally, the assessment tools within economic evaluation provide critical insight into the potential societal impacts of healthcare decisions.
In practice, the integration of economic evaluation requires continuous collaboration among stakeholders in the healthcare sector. These evaluations guide the formulation and refinement of health policies by providing a comprehensive understanding of intervention impacts. With healthcare demands escalating, economic evaluation becomes indispensable in fostering accountable and adaptable health systems.
Future Directions of Economic Evaluation in Health Services
Looking forward, economic evaluation in health services is poised for significant evolution. Enhancements in digital health technology promise to revolutionize data collection and analysis, enriching the accuracy of cost and outcome assessments. These technological advancements are expected to alleviate some of the methodological challenges faced previously and increase the reliability of evaluations.
Moreover, there is a growing emphasis on patient-centered care, calling for economic evaluations to incorporate patient experiences and outcomes more deeply. Tailoring evaluations to reflect patient perspectives will further align these assessments with the holistic goals of healthcare services. Continued investment in training and capacity-building will equip healthcare professionals with the requisite skills to implement economic evaluation in health services robustly.
Conclusion on Economic Evaluation in Health Services
Economic evaluation in health services remains a critical facet of effective healthcare management. By scrutinizing the economic and clinical implications of health interventions, these evaluations ensure that resource allocations are justified and beneficial. Policymakers and healthcare professionals should increasingly rely on economic evaluation to guide sustainable and equitable health system development.
In conclusion, the evolution of economic evaluation in health services continues to expand its role and significance. With growing healthcare demands and finite resources, its application is more vital than ever for securing a future where healthcare delivery is both economically sustainable and optimally effective. Embracing economic evaluations will enable healthcare systems globally to meet these challenges and improve overall healthcare outcomes.