The intricate relationship between healthcare expenditure and patient outcomes is a topic that has garnered significant attention from policymakers, healthcare professionals, and researchers alike. Understanding how financial resources allocated to healthcare influence the quality and effectiveness of patient care is paramount. This article delves into the multifaceted dynamics between healthcare expenditure and the resulting patient outcomes, evaluating the implications of varied spending levels on the overall performance of healthcare systems.
Read Now : Advanced Residue Treatment Processes
The Correlation Between Healthcare Expenditure and Patient Outcomes
Healthcare expenditure is a critical factor in determining the scope and quality of services provided to patients. Higher levels of expenditure may signal better resources for preventative care, advanced medical technologies, and well-trained medical staff, potentially leading to improved patient outcomes. Conversely, excessive expenditure does not automatically equate to enhanced patient outcomes; efficiency and strategic allocation play crucial roles. Despite significant investment, some countries with high healthcare expenditure do not necessarily exhibit superior patient outcomes, underscoring the complexity of this relationship.
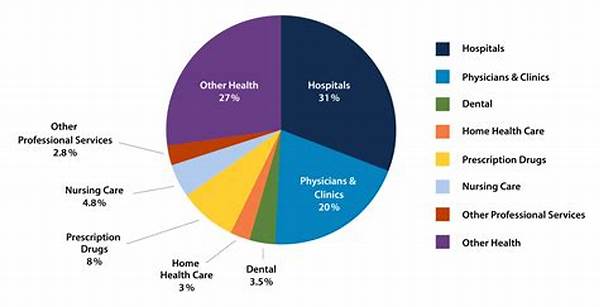
Moreover, the cost-effectiveness of healthcare interventions is an essential consideration in understanding this correlation. While higher spending can stimulate advancements in healthcare delivery and infrastructure, it is imperative to evaluate whether these investments translate into tangible improvements in patient outcomes. Effectively managing healthcare expenditure to optimize patient outcomes remains a substantial challenge, necessitating a careful balance between financial investment and strategic healthcare planning across various sectors.
Key Factors Influencing Healthcare Expenditure and Patient Outcomes
1. Resource Allocation: Strategic resource allocation in healthcare is vital; indiscriminate spending can lead to inefficiencies without improving patient outcomes.
2. Technological Advancements: While technology boosts healthcare, its costs must be managed to ensure positive patient outcomes without unnecessary healthcare expenditure.
3. Preventative Care Investment: Increased focus on preventative care can optimize healthcare expenditure by reducing the need for expensive treatments, thereby potentially enhancing patient outcomes.
4. Workforce Training and Development: Investing in healthcare workforce education improves service delivery efficiency, contributing positively to patient outcomes.
5. Policy and Regulation: Sound healthcare policies and regulations can directly influence the efficacy of healthcare expenditure and thus affect patient outcomes positively.
Impact of Healthcare Infrastructure on Expenditure and Outcomes
The development of healthcare infrastructure is a significant determinant of how healthcare expenditure affects patient outcomes. Large-scale investments in state-of-the-art facilities, equipped with cutting-edge technology, are necessary to provide high-quality care. However, the discrepancy between rural and urban healthcare infrastructures often leads to unequal distribution of resources. As a consequence, patient outcomes can vary significantly based on geographic location, as access to comprehensive healthcare services is not uniformly available.
Moreover, the emphasis on building resilient healthcare infrastructure should also consider the adaptability and preparedness of healthcare systems to respond to emergencies and pandemics. Robust infrastructure facilitates better management of healthcare expenditure by streamlining operations, reducing waste, and promoting efficiency. In turn, this leads to enhanced patient outcomes by ensuring timely and adequate medical attention, reducing complications, and improving recovery rates.
Challenges in Balancing Healthcare Expenditure and Patient Outcomes
Balancing healthcare expenditure and patient outcomes presents numerous challenges. Here are ten critical considerations:
1. Equitable Access: Ensuring equitable access to quality healthcare regardless of income or geographic location.
2. Cost Management: Implementing effective cost control measures without compromising patient care quality.
3. Public Health Objectives: Aligning expenditure with broader public health objectives for comprehensive community well-being.
4. Evolving Medical Needs: Addressing the changing healthcare demands due to demographic shifts and emerging health issues.
Read Now : Evaluating Research Impact Measurement
5. Preventative vs. Curative Focus: Balancing investments in preventative measures against curative treatments.
6. Data and Analytics: Utilizing data analytics to make informed decisions on budgeting and spending in healthcare.
7. Sustainability: Ensuring healthcare expenditure is sustainable, considering economic constraints and health system needs.
8. Patient-Centered Care: Fostering a patient-centered approach in healthcare delivery to optimize outcomes.
9. Innovation Adoption: Carefully integrating innovations that genuinely enhance patient outcomes without unnecessary costs.
10. Quality Monitoring: Implementing systems to monitor healthcare quality to ensure expenditure translates to improved outcomes.
Strategies for Optimizing Healthcare Expenditure and Patient Outcomes
Optimizing healthcare expenditure to enhance patient outcomes requires a multifaceted approach. First and foremost, healthcare systems must prioritize the effective allocation of resources. By focusing on evidence-based strategies, funds can be directed to areas delivering the most profound impact on patient care. Emphasizing preventative care not only aids in reducing the overall burden of chronic diseases but also represents a more cost-effective approach to healthcare.
Furthermore, the integration of technology must be accompanied by comprehensive evaluation frameworks to gauge its impact on patient outcomes. While technological advancements have revolutionized diagnosis and treatment modalities, they should be judiciously implemented to ensure meaningful improvements in patient well-being. Rigorous workforce training and development programs can further augment healthcare delivery by equipping healthcare professionals with the necessary skills to address evolving patient needs, ultimately contributing to better health outcomes.
Innovative Approaches in Expenditure Analysis and Outcome Enhancement
Adopting innovative approaches is essential to bridge the gap between healthcare expenditure and patient outcomes. Predictive analytics, for instance, can aid in understanding future healthcare trends, allowing for preemptive adjustments in budget allocation. Leveraging such technologies ensures that healthcare resources are not only distributed efficiently but also effectively tailored to patient requirements, optimizing outcomes.
Moreover, fostering collaborative initiatives between public and private sectors can enhance resource mobilization and utilization, particularly in addressing complex health challenges. By promoting transparency, accountability, and stakeholder engagement, healthcare systems can achieve a more streamlined expenditure process. This, in turn, aligns financial planning with the overarching goal of improving patient health, thus establishing a sustainable model for future healthcare delivery.
In summary, to optimize healthcare expenditure and improve patient outcomes, there is an urgent need for strategic and innovative initiatives. These entail leveraging technology, fostering public-private partnerships, and implementing rigorous quality monitoring systems. Such measures can ensure that healthcare expenditure is not only judiciously managed but also generates significant, positive impacts on patient outcomes.